Abstract
Aims
Cardiovascular risk factors, such diabetes, hypertension, blood pressure, obesity, and smoking, are linked with allostatic-interoception – the continuous monitoring of internal bodily states in anticipation of environmental demands. These risk factors are associated with dementia risk. How these factors affect brain networks vulnerable to neurodegeneration and involved in allostatic-interoception, such as the Allostatic-Interoceptive Network (AIN), is unknown. We investigated the relationship between cardiovascular risk and AIN structure and function in frontotemporal lobar degeneration (FTLD) and Alzheimer’s disease (AD).
Methods
We recruited 1501 participants (304 with FTLD, 512 with AD, and 685 healthy controls) from the Multi-Partner Consortium to Expand Dementia Research in Latin America (ReDLat). A cardiovascular risk score was calculated based on: age, sex, diabetes, hypertension, systolic blood pressure, body mass index, and smoking status. Cardiovascular risk was associated with gray matter integrity and functional connectivity in age- and sex-matched patient-control groups focusing on predefined regions of interest within the AIN.
Results
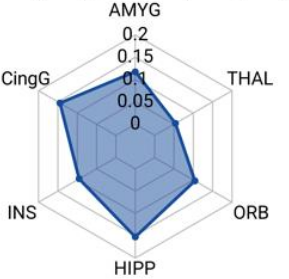
Higher cardiovascular risk was associated with reduced structural integrity and functional connectivity within the AIN in both FTLD and AD. FTLD patients showed more extensive structural and functional connectivity disruptions throughout the AIN. In AD patients, structural reductions in the AIN were prominent, with functional connectivity restricted to the hippocampus, parahippocampal gyrus, and orbitofrontal regions
Conclusions
Cardiovascular risk factors appear to adversely impact the AIN structure and function, with disease-specific patterns of vulnerability. Results underscore the importance of integratingCVR-2025-0447: Cardiovascular risk and allostatic-interoception in dementia cardiovascular health into models of neurodegenerative disease and managing cardiovascular health to support brain integrity in dementia.